Menopause is a natural transition in a woman’s life, typically occurring between the ages of 45 and 55. But for some, this shift begins far earlier. When menopause starts before age 40, it’s considered premature menopause, and when it occurs before age 45, it’s referred to as early menopause.
This change can be unexpected and distressing, especially for women who are still planning for children or are surprised by the symptoms. While aging is the most common cause of menopause, early onset can be linked to several other medical and lifestyle-related factors. Understanding these causes is an important part of protecting long-term health.
What Is Premature Menopause?
Premature menopause refers to the permanent end of menstruation before age 40. It results from the ovaries no longer producing typical levels of estrogen and progesterone, leading to the end of ovulation and menstruation.
The signs are similar to those of typical menopause and may include:
- Irregular or missed periods
- Hot flashes and night sweats
- Mood changes
- Vaginal dryness
- Decreased libido
- Difficulty sleeping
- Memory or concentration problems
Women experiencing these symptoms in their 30s or early 40s should speak with their physician. Premature menopause may affect not only fertility but also long-term cardiovascular, bone, and cognitive health.
Common Causes of Premature Menopause
1. Genetic Factors
In some cases, premature menopause runs in families. If a woman’s mother or sister went through menopause prematurely, there may be a hereditary component at play.
2. Autoimmune Conditions
Certain autoimmune disorders (such as thyroid disease, lupus, or rheumatoid arthritis) can cause the body to attack its own ovarian tissue, affecting hormone production and ovulation.
3. Medical Treatments
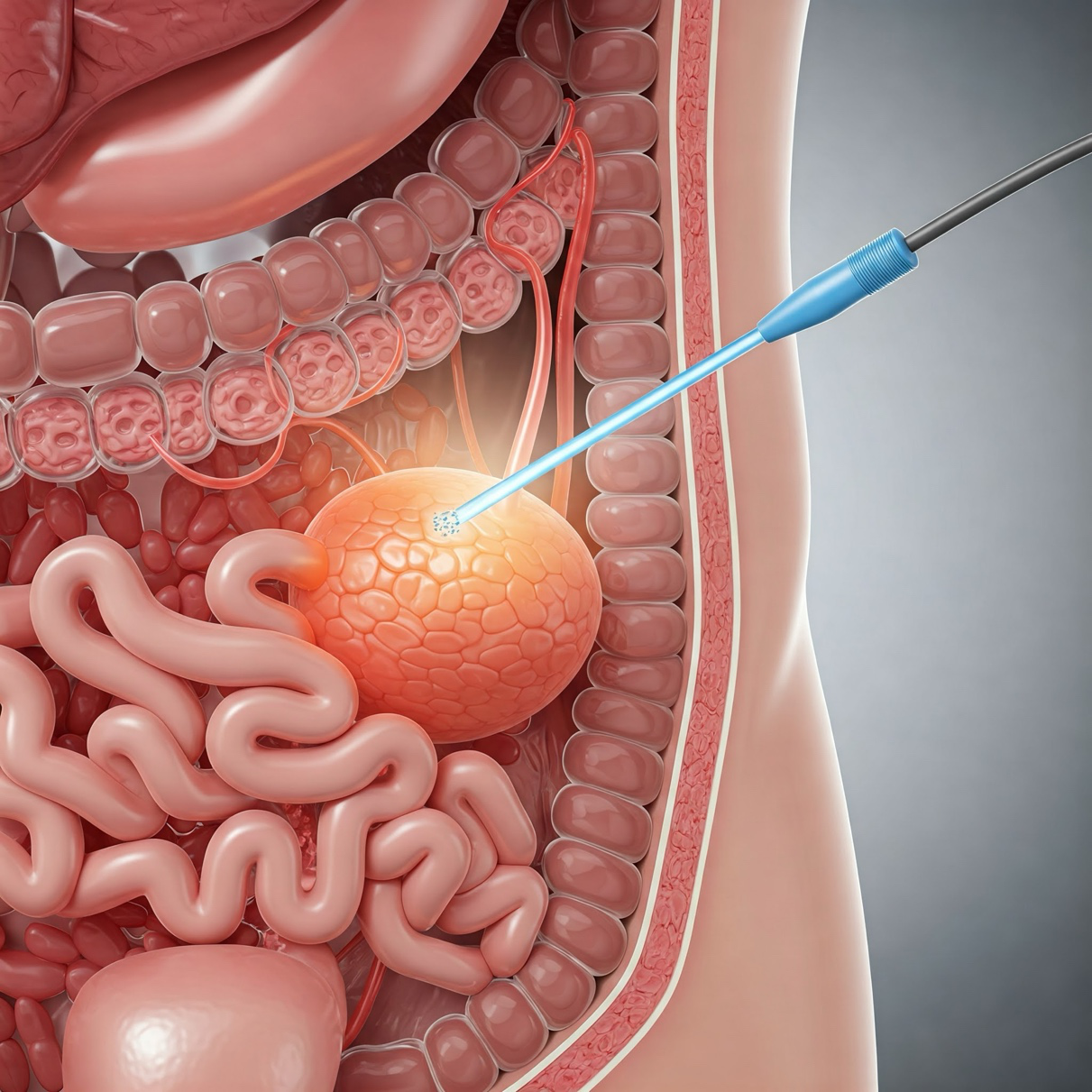
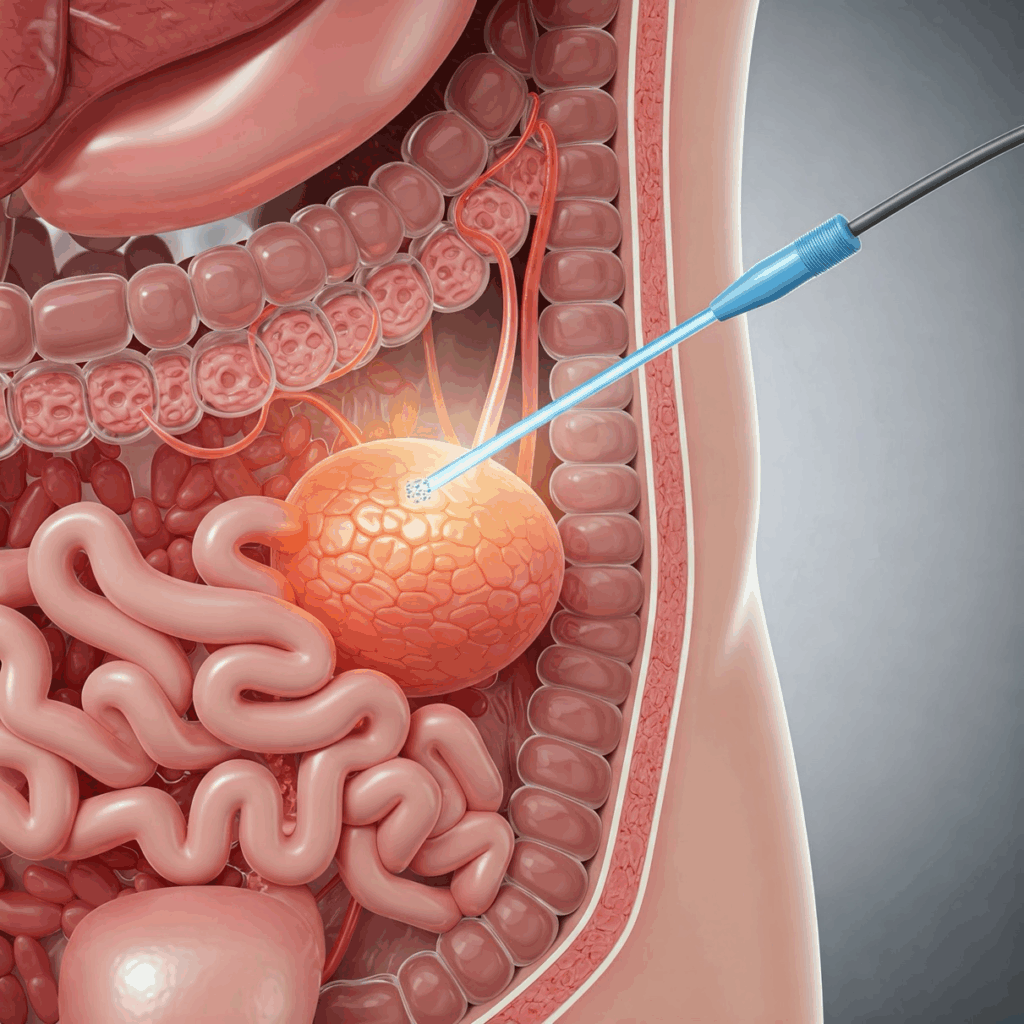
Cancer treatments, especially chemotherapy and pelvic radiation, may damage ovarian function. Similarly, surgical removal of the ovaries (oophorectomy) causes immediate menopause regardless of age.
4. Chromosomal Abnormalities
Genetic conditions such as Turner syndrome or fragile X syndrome can lead to early ovarian failure.
5. Smoking
Research shows that smoking is linked to earlier onset of menopause, likely due to its impact on estrogen levels and ovarian health.
6. Certain Infections
In rare cases, infections like mumps or tuberculosis may affect the ovaries and lead to premature menopause.
7. Idiopathic (Unknown Cause)
In some instances, no clear cause is identified. This is referred to as idiopathic premature menopause and accounts for a significant percentage of cases.
What Can Be Done About Premature Menopause?

While premature menopause is not reversible, there are ways to manage symptoms and reduce health risks.
1. Hormone Therapy (HT)
Estrogen replacement (sometimes combined with progesterone) is commonly prescribed to reduce symptoms and protect against bone loss or heart disease. HT is typically recommended for women with premature menopause until they reach the natural menopausal age, unless contraindicated.
2. Lifestyle Changes
- Bone Health:Calcium-rich foods, weight-bearing exercise, and vitamin D can help maintain bone strength.
- Cardiovascular Health:A heart-healthy diet, regular physical activity, and avoiding smoking support vascular health.
- Mental Well-Being:Counseling or support groups can be helpful, especially if premature menopause affects emotional health or family planning.
3. Fertility Preservation (When Applicable)
For women at risk of premature menopause due to medical treatments (such as chemotherapy), options like egg or embryo freezing may be discussed ahead of time.
4. Regular Screenings
Routine checkups, bone density tests, and heart health screenings are essential for premature menopause patients to monitor and manage long-term risks.
Compassionate Gynecologic Care for Every Stage of Life
The physicians at Houston Physician Hospital are experienced in diagnosing and managing premature menopause and its related health effects.
If you’re noticing symptoms of hormonal change before age 40, don’t wait to seek care. Early evaluation and treatment can make a lasting difference in your health and well-being. On the Gynecology page, you can scroll down and find a gynecologist who’s right for you. Then click their bio to visit their website and make an appointment.